Why lung cancer screening is a glimpse into the future of digital prevention
Last month, a small multi-disciplinary team from the Digital Prevention Services Portfolio (where I am Head of Product for Screening) presented to the NHS England team responsible for Lung Cancer Screening on how we would go about digitising a section of the participant journey.
This section is interesting because, after being invited for screening, the participant answers a few questions about themselves, this information is then used to calculate a risk score, and finally, those who exceed a certain threshold are invited for a CT scan of their lungs to check for abnormalities.
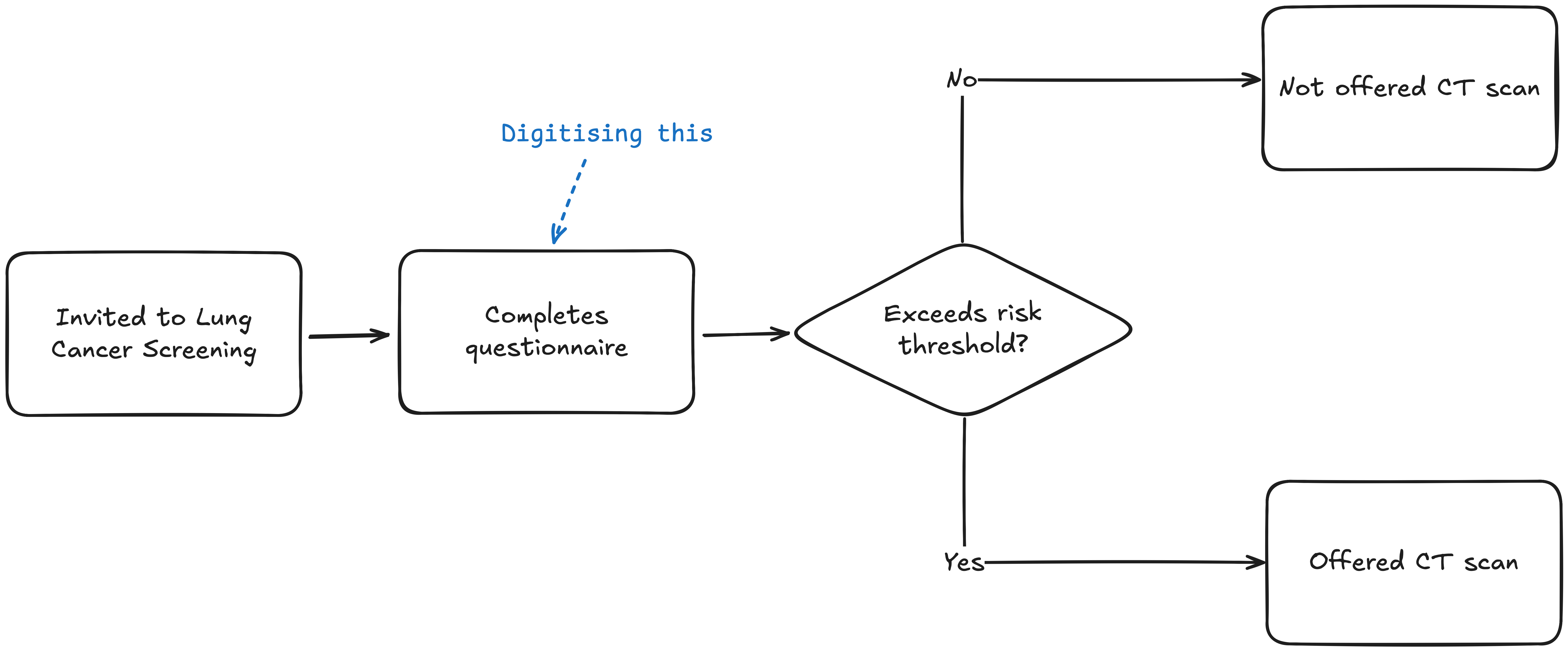
Today, the assessment is carried out over the phone, but our hope is that in the (not to distant) future, participants have the option to complete the assessment online and, should they need to, book a slot for their CT scan online too.
Delivering on this work will provide participants with a different route for completing the assessment, and, for those who choose to use it, it will save the programme money when compared to relatively costly phone consultations. Most importantly however, it supports the delivery of the 10 Year Plan commitment to move Lung Cancer Screening from its current pilot phase into a nationally available offer.
Targeted screening vs. population screening
When someone talks about healthcare screening they are mostly likely talking about a programme like Breast, Bowel or Cervical screening. These are what we call population screening programmes, meaning that the group of people being invited to screening are filtered by age and sex only. However, a targeted programme is different because, as the UK’s National Screening Committee describes, the participants are, “identified as being at elevated/above average risk of a specific condition.”
Currently 10 million people in England are screened every year through the three main population programmes. Uptake of these programmes is a common point of discussion, and, all things equal, more uptake means we will screen more people. But screening people is not without harm. It causes emotional distress, costs money and will inevitably include false positives which lead to unnecessary and invasive procedures. A more radical topic of conversation would be: how do we screen half as many people, while ensuring that we the half we do screen are the most at risk?
Ultimate direction will come from the national regulator. A good thing! You want to be guided by the scientific evidence and not the hunches of some product guy. But those of us building the digital infrastructure to support screening still have a role to play: we must invest in modern digital services that can react quickly to the changing scientific and regulatory landscape; and we must work proactively by analysing, and providing access to, the data we store in order to shape future policy recommendations.
Towards a more responsive future
Take a further step back and you can see not just a model for more effective screening, but the future of preventative healthcare too. In abstract terms, consider, gathering a user’s health data, calculating a score using some risk model, and, finally, provide the user with recommended follow up action. This model could be equally applied to a whole host of healthcare scenarios.
You can see space for innovation at each stage of the value chain too.
In the case of Lung Cancer Screening the health data is a fairly rudimentary participant submitted questionnaire, but I can see a future where this might include family history of a condition, genetic predisposition, information from wearables, clinical observations from primary and secondary care records, etc.
The risk model may get more sophisticated as well. From logistic regression, as in the lung programme, to a machine learning system that can improve over time, or one that uses natural language processing (like a modern chatbot) to make sense of large quantities of unstructured data – we have a lot of unstructured data in the NHS.
How you manage the demand and supply of prevention programmes could change too. From the kind of multi-year cycles we see in screening today, to a system that responds based on near real-time risk calculations and the local availability of the next best action.
This would be a much more responsive model of preventative healthcare, and, if Lung Cancer Screening is anything to go by, it’s not as far off as it might first seem.
Thanks to Sarah Fisher and Giles Turnbull for reviewing drafts of this post.